Winkelwagen
U heeft geen artikelen in uw winkelwagen
Bij het ontstaan van urticaria speelt histamine een belangrijke rol. Histamine ligt opgeslagen in bepaalde cellen (voornamelijk mestcellen) in de huid. Histamine wordt uit deze cellen vrijgemaakt onder invloed van prikkels van uiteenlopende aard. Door het vrijkomen van histamine verwijden bloedvaten zich, waardoor de huid een rode kleur krijgt.
Bovendien veroorzaakt histamine een toegenomen doorlaatbaarheid van vocht door de wanden van de bloedvaten, waardoor vochtophoping ontstaat in de huid. Ook veroorzaakt histamine jeuk.
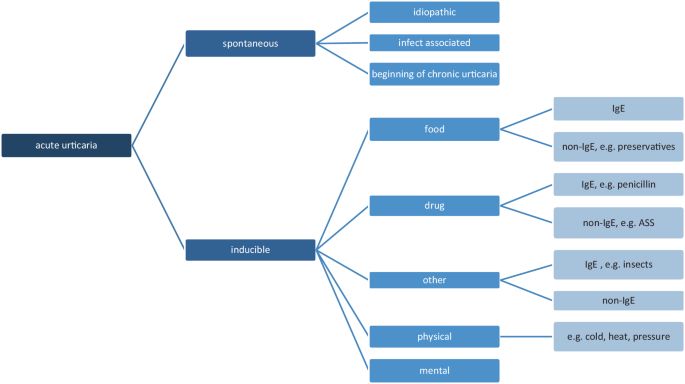
De prikkels, die histamine kunnen vrijmaken, kunnen ingedeeld worden in de volgende groepen:
Soms zijn meerdere prikkels tegelijkertijd aanwezig.
Ook kunnen sommige prikkels reeds bestaande urticaria verergeren, zoals fysische prikkels en pijnstillers.
Bij chronische urticaria kan bij 60-90% van de patiënten geen oorzaak gevonden worden. Men spreekt dan van “chronische idiopatische urticaria”.
Ofschoon er geen duidelijke erfelijke aanleg bestaat, komt urticaria in bepaalde families vaker voor. Dit geldt vooral bij bepaalde vormen van urticaria, zoals koude-urticaria en zonlicht-urticaria.
In-vivo and in-vitro methods are useful in diagnostic evaluation, in addition to history and physical examination. Skin tests are quick to perform and considered relatively safe.
In-vivo test
Prick test: It is considered the test of choice for the diagnosis of ICU. The inner aspect of the forearm is the preferred site, and multiple allergens can undergo testing simultaneously, using positive control with histamine and negative control with normal saline with results interpreted in 30 minutes. False-positive results occur due to a positive reaction from one test site spreading to the neighboring site or irritant reaction. PCD is diagnosable with the prick test. If skin prick tests and serum allergen-specific IgE tests are negative, a provocation or direct challenge test may be needed.
Open test/ skin provocation test: The open test is used for the diagnosis of NICU. The test consists of gently rubbing 0.1ml of the test substance over a 3 cm x 3 cm area of intact skin on the volar aspect of the forearm. The site requires an examination at 20, 40, and 60 minutes. The best vehicle for testing the agents is an alcohol-water or alcohol propylene glycol mixture.
Use test: The test agent in the same vehicle of delivery is used to observe for the reaction. The serial incremental dosing of the agent is. The usual sites of skin testing are the upper back, flexor aspect of the upper arm, and forearm.
Scratch test: A deep dermal scratch with the test substance is performed using the blunt bottom of a lancet after the allergen is applied to the skin, this is useful for diagnosing CU to non-standard allergens.[12] Due to the risk of anaphylaxis, it should always take place under medical supervision.
Intradermal testing: The test uncommon due to the risk of anaphylaxis. When testing with non-standardized substances, the test controls should be assessed on at least 20 people to rule out false-positive results.

No. Whilst other causes of a skin rash are contagious, hives aren't.
Inducible urticaria most commonly occurs in healthy young adults. As a rule, hives triggered by physical stimuli tend to improve and become less troublesome with time (often going, or being much less troublesome, after 2-5 years).
Acute hives usually last less than six weeks. Most cases last 24-48 hours and in some cases the rash only lasts a few hours.
Persistent hives tend to come and go. There may be times when the rash appears on most days, and then times when the rash may go away for a while. The severity of the rash and itch varies from person to person. Some things such as heat, cold, menstrual periods, stress, or emotion may make the rash flare up worse than usual.
Acute spontaneous urticaria, since it is self-limiting, usually does not require any special diagnostic workup besides a history for possible trigger factors. However, a targeted history is important and can lead to useful diagnostic measures.
The history should include the following questions:
In such cases, allergological diagnostics such as prick testing or intradermal testing (especially for drugs available in sterile solution) should be performed. In addition, allergy testing should include determination of specific IgE, in vitro tests (e.g., cellular antigen stimulation test [CAST], basophil activation test [BAT]), and/or exposure testing, if possible and appropriate.
