Winkelwagen
U heeft geen artikelen in uw winkelwagen
The present case provides two clinical messages: 1) early diagnosis and treatment are crucial for a favorable outcome after adrenal failure following adrenal haemorrhage, and 2) we emphasize the importance of careful observation of the patient with autoantibodies, LA and ANA, because autoantibodies precede clinical manifestations of autoimmune diseases, such as SLE [9].
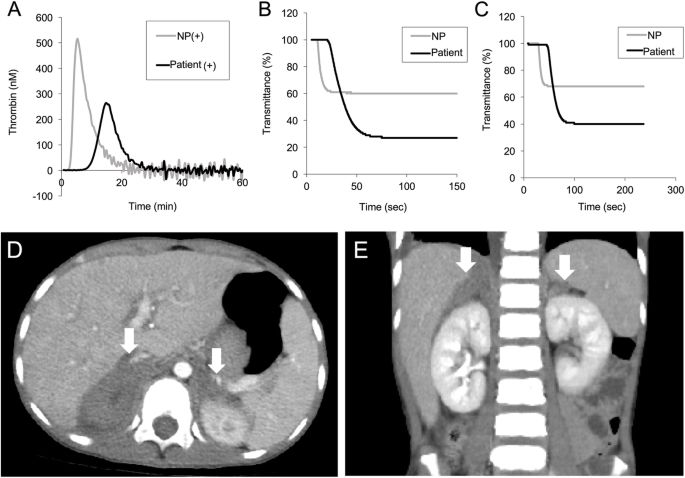
LAHPS is mainly found in children with LA and is accompanied by a decrease in plasma prothrombin activity due to IgM class anti-prothrombin antibody [3, 4]. LAHPS was reported by Bajaj in 1983, and the pathophysiology of LAHPS is thought to be an immune complex with prothrombin antibody, which is rapidly excreted from the blood, resulting in low prothrombin activity [10]. In our case, a decrease in prothrombin activity supports a similar pathophysiology. LAHPS-associated adrenal haemorrhage is rare, however, paediatricians should pay attention to this complication for unexplained or prolonged abdominal pain.
Adrenal failure due to adrenal haemorrhage is rare, but potentially fatal [6, 11]. In childhood, it generally presents with nonspecific signs and symptoms, such as fatigue, malaise, abdominal pain, nausea, and vomiting, without hyperpigmentation. Therefore, diagnosis and treatment may often be delayed. Our case showed prolonged abdominal pain and deranged coagulation, and early recognition of adrenal insufficiency due to adrenal haemorrhage enabled early intervention. The pathophysiology of adrenal gland bleeding remains unclear. The adrenal gland comprises a rich arterial supply with a single vein limiting blood drainage, a thrombosed vein can result in progressive increase in arterial blood pressure [12].
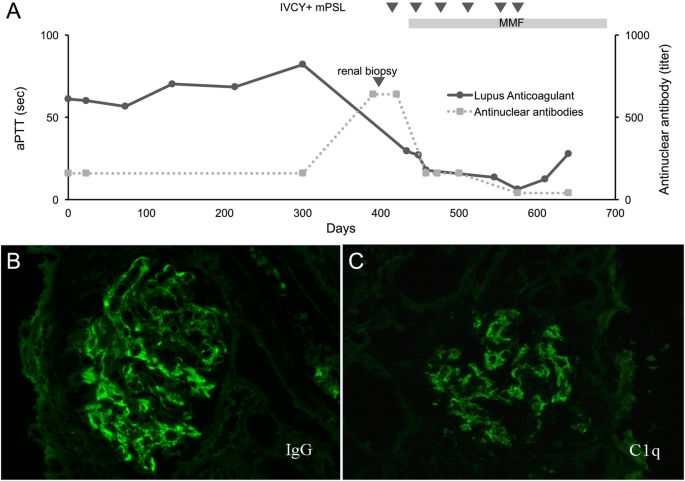
Antibodies promoting thrombosis are known to be associated with autoimmune diseases, such as antiphospholipid syndrome, or to be produced in reaction to an acute infection, particularly in children [13, 14]. However, our patient developed SLE after 1 year, a development described less frequently than the opposite one [9, 15]. Moreover, the patient did not fit the SLICC diagnostic criteria for SLE, nor is haemorrhage, with the partial exception of alveolar haemorrhage, a typical presentation of SLE. However, autoantibodies, including LA and ANA, persisted [16]. The development of autoantibodies has been reported to precede clinical manifestations of autoimmune diseases, such as SLE [9]. Renal dysfunction was also observed when SLE was diagnosed in our case. Therefore, we emphasize that the finding of autoantibodies in a patient with coagulation disorders should be followed by long-term monitoring.
Simanek R, Panzer S, Lechner K, Pabinger I. Late spontaneous remissions in severe adult autoimmune thrombocytopenia. Ann Hematol. 2007 Oct, 86 (10):705-10. [PubMed : 17503045 ]
Hell L, Ay C, Posch F, Gebhart J, Koder S, Mackman N, Pabinger I, Thaler J. Low extracellular vesicle-associated tissue factor activity in patients with persistent lupus anticoagulant and a history of thrombosis. Ann Hematol. 2019 Feb, 98 (2):313-319. [PMC free article : PMC6342892 ] [PubMed : 30467688 ]
Tripodi A. Laboratory testing for lupus anticoagulants: a review of issues affecting results. Clin Chem. 2007 Sep, 53 (9):1629-35. [PubMed : 17712001 ]
Galli M, Luciani D, Bertolini G, Barbui T. Lupus anticoagulants are stronger risk factors for thrombosis than anticardiolipin antibodies in the antiphospholipid syndrome: a systematic review of the literature. Blood. 2003 Mar 01, 101 (5):1827-32. [PubMed : 12393574 ]
de Laat HB, Derksen RH, Urbanus RT, Roest M, de Groot PG. beta2-glycoprotein I-dependent lupus anticoagulant highly correlates with thrombosis in the antiphospholipid syndrome. Blood. 2004 Dec 01, 104 (12):3598-602. [PubMed : 15315975 ]
Devreese K, Peerlinck K, Hoylaerts MF. Thrombotic risk assessment in the antiphospholipid syndrome requires more than the quantification of lupus anticoagulants. Blood. 2010 Jan 28, 115 (4):870-8. [PubMed : 19965629 ]
Favaloro EJ, Mohammed S, Curnow J, Pasalic L. Laboratory testing for lupus anticoagulant (LA) in patients taking direct oral anticoagulants (DOACs): potential for false positives and false negatives. Pathology. 2019 Apr, 51 (3):292-300. [PubMed : 30665674 ]
Love PE, Santoro SA. Antiphospholipid antibodies: anticardiolipin and the lupus anticoagulant in systemic lupus erythematosus (SLE) and in non-SLE disorders. Prevalence and clinical significance. Ann Intern Med. 1990 May 01, 112 (9):682-98. [PubMed : 2110431 ]
Dembitzer FR, Ledford Kraemer MR, Meijer P, Peerschke EI. Lupus anticoagulant testing: performance and practices by north american clinical laboratories. Am J Clin Pathol. 2010 Nov, 134 (5):764-73. [PubMed : 20959659 ]

Lupus anticoagulant-hypoprothrombinemia syndrome (LAHPS) is characterized by bleeding and thrombosis in patients with autoimmune diseases or infections. Paediatric LAHPS exhibits various degrees of bleeding, ranging from mild to severe, however, adrenal haemorrhage due to LAHPS and its long-term clinical course have not been sufficiently described.
A 9-year-old boy presented with prolonged abdominal pain and abnormal coagulation screening tests. The laboratory tests showed prolonged activated partial thromboplastin time and subsequently revealed the presence of lupus anticoagulant, anti-nuclear antibodies, and hypoprothrombinemia, leading to diagnosis of LAHPS. An enhanced computed tomogram demonstrated nodular lesions in the adrenal glands bilaterally, suggestive of adrenal haemorrhage. Laboratory and clinical manifestations exhibited life-threatening adrenal insufficiency that required hydrocortisone administration. The patient developed systemic lupus erythematosus, diagnosed 12 months later.
This patient with LAHPS developed rare adrenal failure due to adrenal haemorrhage, a life-threatening event that should be recognized and treated early. In our case, renal dysfunction was also observed when systemic lupus erythematosus was diagnosed 1 year after LAHPS. Our case emphasizes that early recognition of adrenal failure and careful long-term observation is required in patients with autoantibodies.