Winkelwagen
U heeft geen artikelen in uw winkelwagen
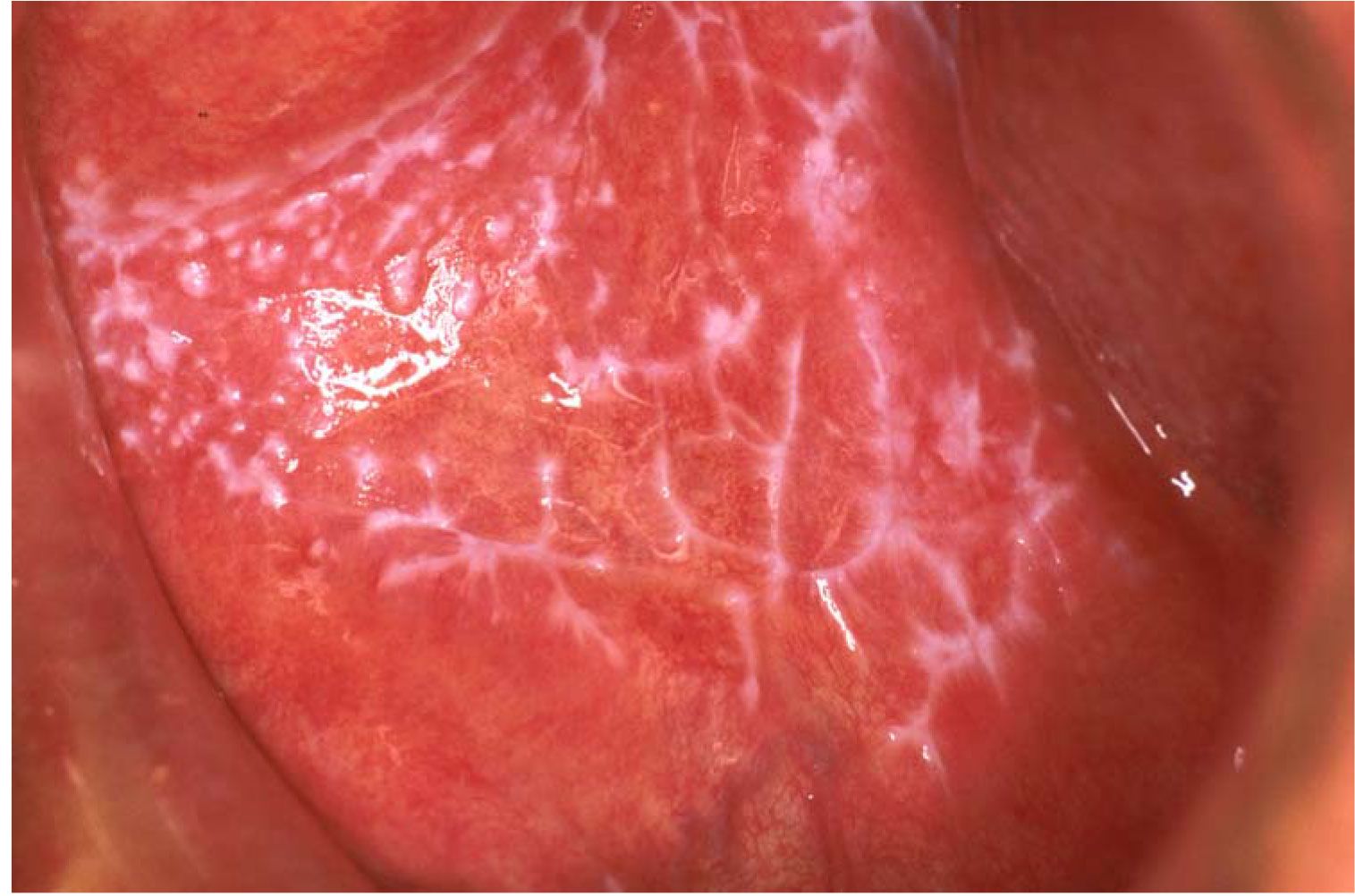
There are six clinical subtypes of OLP: reticular, papular, plaque, atrophic, erosive, and bullous.[30] These may be present either individually or in combination with each other, and the classification is usually based on the predominant subtype manifested.[21]
An accurate diagnosis of OLP must be based on thorough history taking, clinical examination, and histopathologic findings. In patients presenting with the characteristic reticular form of OLP, the clinical presentation alone can be sufficiently diagnostic. However, an oral biopsy is still advisable to confirm the clinical diagnosis and to rule out evidence of dysplasia and malignancy.[29]
For patients who present with desquamative gingivitis, direct immunofluorescence (DIF) may be necessary to rule out autoimmune vesiculobullous diseases that share similar clinical features.[19]
Diagnosis of OLP is challenging because of the presence of overlapping clinical and histopathological features. The diagnosis of an OLP may be made on visual examination without any biopsy when the lesion presents with the characteristic Wickham's striae.[24,25] A complete history and clinical assessment by various specialists such as dermatologist, ophthalmic surgeon, general physician and gastroenterologist may be required to investigate the involvement other than oral cavity.
The investigations include (1) cytology, (2) hematology and (3) biopsy (histopathological and immunofluorescence).
Smear examination is mandatory in a desquamative lesion and Tzanck test is a simple, fast and inexpensive diagnostic test that can be performed with minimal patient discomfort that is used in erosive lesion, especially on the gingiva to identify the presence of acantholytic cells [ Figure 17 ] and to rule out pemphigus vulgaris. Cytology is also helpful to distinguish the presence or absence of hyphae by doing a direct potassium hydroxide stain and or by culture in Sabouraud dextrose agar media [ Figure 18 ]. Monitoring the development of candidiasis during the treatment while administering the topical steroids may be helpful toward a successful treatment [ Figure 19 ].
Sabouraud dextrose agar
Candidiasis following steroid application

Histopathology of oral lichen planus
It was First described by DUHRENILL in 1906 and later revised by SHKLAR in 1972:[25,27]
Hyperkeratosis of surface epithelium (orthokeratosis or parakeratosis)Max Joseph spaces which are histological clefts between basement membrane lamina and propria interface caused due to liquefaction necrosis of basal layer
Juxta-epithelial band of inflammatory cells predominantly T-lymphocytesCivatte/hyaline/cytoid/colloid bodies which are Degenerating keratinocytes at the epithelial connective tissue interface
An eosinophillic band may be seen just beneath the basement membrane and represent fibrin covering lamina propria.

This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
OLP is defined as a common chronic immunological mucocutaneous disorder that varies in appearance from keratotic to erythematous and ulcerative (Wilson 1896)[6]
Lichen planus is a relatively common disorder of the stratified squamous epithelia (Duske and Frick, 1982: Skully and El-kom 1985)[7,8]
OLP as a relatively common chronic inflammatory disorder affecting the stratified squamous epithelia[7]
Lichen planus is a common disorder in which auto-cytotoxic T-lymphocytes trigger apoptosis of epithelial cells leading to chronic inflammation. OLP can be a source of severe morbidity and has a small potential to be malignant (Scully et al. 2008).[8]

In 1978, WHO formulated diagnostic criteria for OLP, which included both clinical and histopathological features for consideration.
White papular-, reticular (lace-like network of slightly raised gray-white lines), annular- or plaque-type lesions
Presence of a well-defined band like zone of cellular infiltration that is confined to the superficial part of the connective tissue, consisting mainly of lymphocyte
Signs of “liquefaction degeneration” in the basal cell layer.He considered some essential criteria for diagnosis that includes:
Band-like lymphocytic infiltrate at the epithelial–stromal junction, with obfuscation of the basal cell region
He suggested some features to be excluded:
Atypical cytomorphologies (suggestive of epithelial dysplasia) – hyperchromasia, prevalent dyskeratosis and increased mitotic figures
Heterogeneous population of inflammatory infiltrate, deeper submucosal extension of infiltrate beyond superficial stroma and perivascular infiltration.